Coming soon:
To keep up to date with future webinars, check our website or sign up to our newsletter.
See the videos of recent webinars below.
Coproduction – being an effective lived-experience partner
26 October 2023
- Are you someone with lived experience of musculoskeletal conditions?
- Would you like to know how to be involved in the design of MSK services?
Increasingly the NHS is realising the importance of talking to the people who use their services about how to do things better. This can be a simple survey, but can also involve focus groups or directly involving people with lived experience in decision making meetings.
If this sounds like something you would like to do but you aren’t sure how to make your voice heard, this webinar is for you.
You will hear:
- More about the different ways people can be involved and what coproduction means.
- What it’s like to be involved and tips for making the best use of the opportunity.
- What managers of NHS services want and why they value hearing from you.
UCB Pharma have provided funding for this initiative. UCB has not influenced or been involved in development of the content of the initiative.
Understanding musculoskeletal health for social prescribing
30 January 2023
Social prescribing services and link workers have the potential to make a big difference to the lives of people with musculoskeletal conditions such as arthritis or back pain. This webinar aims to help you understand musculoskeletal (MSK) conditions, their prevention, their impact, and how to consider this when you meet clients.
Healthy bones, joints and muscles are fundamental to our ability to move, be active, work and engage in activities we enjoy. MSK health underpins our ability to live healthy and independent lives. MSK conditions are the single biggest cause of years lived with disability in the UK and the resulting pain and lack of mobility can have a huge impact on a person’s life.
This webinar is aimed at social prescribing services and link workers, NOT MSK professionals. It’s aimed at people without a detailed knowledge of MSK conditions and will help you know how best to support people living with such conditions. It covers:
- Common MSK conditions and their impact on daily life
- Self-management – what helps including physical activity, diet, weight and daily activities
- Mental health
- Work and education
- What patient organisations can offer
- A social prescribing perspective
This webinar is designed to complement ARMA’s guide for link workers and social prescribing services.
Resources:
The slides to accompany the webinar are available here:
Social prescribing – The benefits, St Helens Wellbeing Service, Sarah Holden (click to open pdf)
MSK conditions and self-management, Arthritis Action, Dr Wendy Holden (click to open pdf)
Social-Prescribing, Arthritis Action, Shantel Irwin, CEO (click to open pdf)
ARMA would like to thank Arthritis Action for their support of this webinar.
The role of patient organisations in rheumatology and implementing the GIRFT rheumatology report
22 October 2021
The recently published GIRFT report on rheumatology found wide variations in rheumatology services and highlights the challenges faced by many units, including rising demand for services, limited resources and an overstretched workforce. The report makes a series of recommendations for changes which would improve patient experience and patient outcomes.
ARMA believes that patient organisations could play a much greater role in supporting these changes than the report indicates. In this webinar, the Chief Executives of two patient organisations outline their vision of the place of patient organisations and how putting their organisations at the heart of the system can help deliver improved services and relieve the pressure on staff.
Support for patients
Clare Jacklin, CEO of National Rheumatoid Arthritis Society, outlines the resources provided to patients by NRAS and how these can help improve patient experience and outcomes.
See the presentation slides to accompany this section of the webinar.
Service improvement
Dale Webb, CEO of National Axial Spondyloarthritis Society, describes how NASS are leading improvements in services and working to reduce delays in diagnosis of AxSpA through their Aspiring to Excellence and Gold Standard programmes.
Between them, Dale and Clare discuss how and why all those identified as responsible for implementing the GIRFT rheumatology report recommendations, nationally and locally, should be engaging with patients and patient organisations at every stage.
Who should watch?
All those identified as responsible for implementing the GIRFT rheumatology recommendations including rheumatology teams, ICSs, commissioners, service managers, those involved in regional networks and service reconfiguration.
This webinar has been sponsored by AbbVie. AbbVie has had no input into the content of the webinar.
Services to support people to live well with pain
17 September 2021
Around one person in three experiences chronic pain and for one person in ten that pain significantly interferes with their daily activities. Designing and delivering effective services and support for these people is a significant challenge.
This webinar will hear from two people who have worked to improve and integrate local pain services.
Between them they will cover:
- Delivering community pain services and living well support.
- Building links between services with a common goal to enable patients living with pain to live a more valued life.
- Embedding health coaching and other psychologically informed approaches ‘upstream’ in the individuals’ journey to reduce demand within pain services, improving access for those who need more specialist pain management support.
- Dialogue and relationship building to drive integration including with IAPT, secondary psychology services, MSK triage and social prescribing.
- Ensuring services will meet specific local population needs.
- Useful resources.
Presenters:
- James Watson, Physiotherapy Pain Lead, Integrated MSK and Community Pain Management, North Tees and Hartlepool NHS Foundation Trust
- Mohammad Shoiab, Pain Specialist Physiotherapist/Clinical Lead, Connect Health Pain Services
Who should watch?
Commissioners, service managers and anyone wanting to improve pain and MSK services; ICS MSK leads; anyone involved in implementing the Best MSK Health programme.
This webinar is part of the ARMA pain programme which is funded in-part through a charitable donation from Pfizer Ltd. Pfizer have had no say in the content of the programme.
Women and Axial Spondyloarthritis: diagnosis and management
9 October 2020
Men with Axial SpA are more likely than women to experience changes to the bones and fusion, and thus they can be picked up using x-ray. Women are more likely than men to experience inflammation rather than fusion, which is visible on MRI but not on x-ray.
In this webinar, three consultant rheumatologists consider what this means for diagnosis and management the evidence, research and case studies. It also considers issues related to pregnancy and co-morbidities.
Who should watch:
GPs, First Contact MSK Practitioners, rheumatologists, ophthalmologists, dermatologists, gastroenterologists, physiotherapists, anyone managing patients with back pain.
The needs of children with inflammation/pain and their families in the context of coronavirus
5 June 2020
The last month has seen a lot of focus on immediate responses to the coronavirus outbreak – assessing a patient’s risk in relation to the virus; which services can be suspended and which need to continue; how to deliver online appointments. What are the differences when considering children and their families in a healthcare setting at this and other times?
In this webinar a parent, rheumatologist and specialist nurse discuss these issues and how services might best respond.
The webinar is aimed at anyone working with paediatric rheumatology patients including rheumatologists, nurses, physiotherapists, paediatricians, GPs, and managers of paediatric services. It is for those who want to explore approaches, ideas, dilemmas and solutions and learn how we can make sure we hear the paediatric voice in these unprecedented times.
Presenters:
Emily Earle, parent and CCAA
Nick Wilkinson, Paediatric Rheumatologist, Guys and St Thomas’ NHS Foundation Trust
Specialist Nurse – tbc
Slides:
The slides to accompany the webinar are available here:
Supporting families living with a long-term paediatric rheumatological condition in the context of the Covid-19 pandemic (click to open pdf)
Introduction to Paediatric and Adolescent Rheumatology (click to open pdf)
Paediatric rheumatology: lived experience and psychological needs
27 March 2020
Around 12,000 children and young people in the UK have a musculoskeletal condition. Supporting them to live the lives they want is an important part of treating their conditions. This webinar explores these issues using the example of Juvenile Dermatomyositis (JDM), a rare condition affecting just 3 in a million children in the UK.
Polly Livermore is a rheumatology nurse who has studied the psychological needs of children with JDM. The findings of her study will be widely applicable to children with other musculoskeletal conditions and many other rare chronic conditions in childhood.
Polly discusses her findings with Clinical Scientist Dr Claire Deakin and a parent, Mrs Carolyn Farrugia.
The webinar covers:
- Paediatric Rheumatology with introduction to Juvenile Dermatomyositis (JDM)
- The UK wide registry which collects data on these children and young people
- What we know about the lived experience and psychosocial needs of children with Juvenile Dermatomyositis and what support they feel they need.
- Current psychology service provision around the UK
- Ideas for future work
Who should watch:
Rheumatologists, nurses, psychologists, allied health professionals, social workers, GPs and any other healthcare professionals working with children and young people with musculoskeletal conditions, voluntary organisations and school teachers.
Presenters:
Polly Livermore, NIHR Clinical Nursing Doctoral Research Fellow, GOSH BRC Clinical Academic Lead at Great Ormond Street Children’s Hospital, NHS Foundation Trust;
Dr Claire Deakin, Senior Scientist, University College London Hospital;
Lyn Farrugia, parent.
What everyone working with back pain needs to know about Cauda equina syndrome
21 February 2020
Cauda equina syndrome (CES) is a rare condition that affects the nerves in the spine supplying the bladder, bowel and sexual function. Identification and subsequent urgent action is required to avoid permanent damage to these essential organs.
Delays in diagnosis can have devastating and life changing consequences for patients and result in high cost negligence claims.
This webinar will be of interest to any health professional treating patients with low back pain, particularly those seeing this patient group in pre-surgical settings. We cover:
- Definition of Cauda Equina Syndrome
- Presenting Signs and symptoms
- Examination for CES
- Evidence relating to CES
- Pathways of Care
- Medico-legal issues relating to CES
Open and save the slides for this presentation. [pdf, 4.4MB]
Who should watch:
Clinicians, physiotherapists, osteopaths, chiropractors, nursing staff, in fact anyone likely to come in to contact with people with back pain.
Presenters:
Laura Finucane, Consultant Physiotherapist, Sussex MSK partnership
Chris Mercer, Consultant Physiotherapist, Western Sussex Hospitals Trust

The Musculoskeletal Association of Chartered Physiotherapists (MACP) is a membership organisation of physiotherapists who have reached a recognised standard of excellence in musculoskeletal physiotherapy. We work to support physiotherapists managing people with musculoskeletal complaints and conditions in a range of settings (NHS, private practice, sport etc.). Our members promote excellence in musculoskeletal health and offer specialist musculoskeletal physiotherapy practice across the UK, with many working as first contact practitioners given their skills and expertise.
For more information about the MACP and how to join visit www.macpweb.org
The Transformation of MSK Physiotherapy Services – a practical example
17 January 2020
General practice in Midlothian is currently experiencing considerable capacity and sustainability challenges, with MSK making up a significant proportion of this demand. Half the practices were operating with restricted lists as a result of increasing demand: a demand which is predicted to quickly rise as the influx of new housing has resulted in Midlothian being the fastest growing local authority area in Scotland.
The transformation of physiotherapy services aimed to address some of these challenges. The webinar covers:
- An overview of the changes we have made within MSK physiotherapy over the last 2 years
- The introduction of first contact physiotherapists as an alternative to a GP for MSK conditions
- The role of the core MSK rehabilitation team
- Challenges we have encountered along the way
- Where we are now and next steps.
Presenters:
Debbie Crerar – Lead Physiotherapist, Midlothian Health and Social Care Partnership
Jennifer Mulvey – Advanced Physiotherapy Practitioner in Primary Care, Midlothian Health and Social Care Partnership
Care and support planning for people with MSK conditions
13 December 2019
The national ambition, set out in the NHS Mandate, is for everyone with a long-term condition to be offered a personalised care plan. This webinar shows how this can be done for with musculoskeletal conditions.
Year of Care Partnerships has worked in collaboration with Versus Arthritis and primary care teams to work out how to include people living with MSK conditions in routine care and support planning (CSP) within the primary care setting. This webinar focuses on the learning and practical issues arising from this study. In particular, we have:
- Described what care and support planning is and how it works in practice;
- Outlined the work involved to include people with MSK conditions within CSP processes;
- Discussed the learning, challenges and potential benefits of working in this way.
You can read the final study report from the versusarthritis.org website.
Who should watch:
Anyone interested in learning more about CSP for people with MSK conditions and how to implement it, including clinicians, primary care team, commissioners, general practice teams etc.
Presenter:
Nick Lewis-Barned, Consultant Physician, Diabetes and Endocrinology, Northumbria Diabetes Service and Clinical Lead, Year of Care Partnerships.
Rheumatology follow-ups: Transforming Outpatients
29 November 2019
The NHS Long Term Plan states that: “Outpatient services will be fundamentally redesigned,” and commits to reducing face-to-face outpatient appointments by up to a third over the next five years.
What does this commitment mean for rheumatology? For rheumatic diseases, long term follow up is often required. However, routinely scheduled appointments mean that patients have to attend hospital even if their symptoms are currently well managed and are not always able to get the support they need when their condition worsens.
This webinar is an opportunity to hear examples of different approaches to rheumatology follow ups and to discuss how to make these services work best for patients and clinicians.
What the webinar covers:
- Learning from two decades of patient initiated follow up (Direct Access) for rheumatology patients at University Hospitals Bristol NHS Foundation Trust.
- The impact of service redesign for rheumatology in South East London, including telephone consultations and AHP review.
- Improving visibility of disease changes as enabling personalised care through integrating the Remote Monitoring of RA app with the electronic patient record at Salford Royal NHS Foundation Trust.
Who should watch:
All those involved in elective care redesign, rheumatologists, rheumatology nurses, rheumatology AHPs.
Presenters:
- Tracy French RGN, MSC, NMP, Rheumatology Clinical Nurse Specialist, University Hospitals Bristol NHS Foundation Trust
- Miranda Willis, South East London Integrated Contract Delivery Team, South East London Commissioning Alliance
- Will Dixon, Professor of Digital Epidemiology and Honorary Consultant Rheumatologist, The University of Manchester and Salford Royal NHS Foundation Trust
The NHS Long Term Plan and rheumatoid arthritis: addressing unmet need
4 November 2019
Whilst care for the over 400,000 people diagnosed with rheumatoid arthritis (RA) has improved over recent years, there are still high levels of unmet need and patients not receiving optimal treatment and support.
Effective implementation of the NHS Long Term Plan should lead to improved care for people with RA. Better patient access to evidence-based treatment, access to multidisciplinary teams in the community, shared decision making, self-management and mental health support all form part of the picture.
This webinar covers:
- Where inflammatory arthritis and RA fit with the NHS Long Term Plan.
- Why early access to therapies to prevent disease progression is important.
- The importance of peer support, self-management support and integrated services and what patient groups have to offer.
Who should watch:
Commissioners and service transformation leads working on MSK pathways, development of community services, and interface between primary and secondary care. PCN and CCG leads on social prescribing, shared decision-making and self-management support. Clinicians in any setting who see patients with RA.
ARMA webinars are free to access thanks to the support of our partners. We would like to thank Abbvie for supporting this webinar. Abbvie have had no say in the content of the webinar.
Speakers:
Dr James Galloway, clinical lecturer at King’s College London and honorary consultant in rheumatology at King’s College Hospital.
Dr Gavin Clunie, Consultant Rheumatologist and Metabolic Bone Physician, Addenbrookes Hospital
Ailsa Bosworth, National Patient Champion, National Rheumatoid Arthritis Society (NRAS)
IAPT and psychological Support for people with MSK conditions
27 September 2019
Pain, mental health and musculoskeletal conditions are strongly linked. Depression is four times more common among people in persistent pain compared to those without pain, for instance. So not recognising or treating one can impact the others greatly.
The Improving Access to Psychological Therapies (IAPT) programme began in 2008. IAPT services provide evidence based treatments for people with anxiety and depression. NHS England is now expanding IAPT services, including introducing IAPT for long term conditions. Some IAPT services now have an offer for people with MSK conditions and pain.
Watch this webinar to hear from two IAPT services that support people with MSK conditions. It includes:
- An introduction to IAPT
- What IAPT has to offer people with MSK conditions and pain
- Early experiences of offering this service
- How IAPT MSK integrates with physical health services
- Commissioning IAPT MSK
Who should watch:
Everyone involved in treating people with MSK conditions, commissioners, IAPT providers.
Presenters:
Dr John Pimm, Head of Service IAPT, Oxford Health NHS Foundation Trust.
Jonny Wilkins, Clinical Team Lead, TALKWORKS – Talking Health, Devon Partnership NHS Trust
Sue Pike, Clinical and Service Manager (Devon), TALKWORKS – Talking Health, Devon Partnership NHS Trust
What a First Contact MSK Practitioner can do for you
20 September 2019
The NHS Long Term Plan aims to see every patient with a musculoskeletal condition have access to a First Contact Practitioner (FCP) by 2023/24. The aim is to provide faster access to diagnosis and treatment and to support more patients to self-manage their conditions. What does implementation of FCP mean for local health systems? What needs to be in place to gain the maximum benefit?
This webinar outlines the basic principles behind FCP. Two presenters who work in areas which have established effective FCP services describe the impact it has had on their work, the benefits of the system and give tips on how to make the best of the changes.
Who should watch:
Commissioners, health care practitioners who see MSK patients, MSK service managers and transformation leads. It will be of particular interest to those in areas which are new to FCP or don’t currently have a service. The webinar is not aimed at First Contact Practitioners.
Presenters:
Benefits of FCP Sarah Withers, Head of FCP Implementation, Chartered Society of Physiotherapy;
First Contact MSK in Gosport Dr Robin Harlow, Clinical Director, The Willow Group of GP Practices;
What an FCP can do for you Rebecca Keating, Planned Care Commissioning Manager, Somerset Clinical Commissioning Group.
Addressing the burden of rheumatic and musculoskeletal foot and ankle pain
10 May 2019
Although foot and ankle pain affects an estimated 20% of the general population and this figure rises to around 90% in people with rheumatoid arthritis, they are frequently trivialised and overlooked. Podiatry and foot health services should, therefore, be a vital part of all MSK and rheumatology services but all too often that’s not the case.
This webinar explores the role of podiatry in multidisciplinary rheumatology & MSK teams and provides examples of how foot health needs can be provided within clinical pathways.
The first presentation by Dr Mike Backhouse (University of York) summarises the latest evidence regarding access to foot care services, serves as an update on the latest guidelines, and provides examples of different models for delivering foot health services. Prof Cathy Bowen (University of Southampton) then examines the early findings from a systematic review of guidelines for the management of foot health. She discusses her recent analysis of the UK GP database of encounters and referrals for foot pain and arthritis. She also presents common themes emerging from interviews with GPs and commissioners, patients, and podiatrists and considers how foot health can be addressed in MSK pathways.
Who should watch:
The webinar is aimed at commissioners and managers of MSK services and everyone involved in treating patients with MSK conditions affecting foot health.
Presenters:
Dr Mike Backhouse, Research Fellow, University of York
Dr Mike Backhouse has a background in podiatry having qualified from the University of Southampton, and over a decade of experience in applied clinical research. His research is highly multidisciplinary and ranges from large pragmatic clinical trials to imaging and mechanism of action studies, all of which aim to improve the lives of people with musculoskeletal disease and other long term conditions.
Prof. Catherine Bowen, NIHR Fellow / Professor in Podiatry, University of Southampton
Professor Catherine Bowen has a specific education and research focus related to investigation and management of inflammatory and non-inflammatory arthritic manifestations within the foot and ankle. Catherine currently holds a UK NIHR Fellowship award investigating optimal models of foot care for individuals who have osteoarthritis (OA). As Professor in Podiatry at the University of Southampton and Honorary Lecturer at the University of Oxford, Catherine leads a multi-professional research partnership with a focus on MSK foot and ankle pathology.
Managing women of child bearing potential living with chronic inflammatory rheumatic disease
3 April 2019
This webinar covers why it is important to appropriately plan a patient’s pregnancy journey, to minimise disease activity to ensure an optimal outcome for mother and baby, and how healthcare professionals can ensure they initiate conversations around family planning at an early stage.
Disease onset for patients living with chronic inflammatory disease (RA, PSA, axSpA and PSO), tends to overlap with peak female reproductive ages. Currently, many women receive inconsistent advice regarding family planning and treatment options during pregnancy. It is important to plan with patients early on and to initiate the discussions even if the patient is not currently planning to get pregnant.
High-disease activity and certain medications (such as NSAIDs and high-dose corticosteroids) have been shown to affect fertility. Active disease is also associated with an increased risk of complications. Adequate disease control before and during pregnancy is crucial to ensure the best maternal and foetal health. Patients who are well controlled during pregnancy are in an optimal position to prepare for birth and breastfeeding.
The webinar covers:
- Current challenges of family planning within this patient group.
- The need to encourage earlier family planning discussions between patients and health care providers, even if the patient is not currently planning to get pregnant.
- The importance of controlling the symptoms of disease/activity before, during and after pregnancy, to ensure optimal outcomes for mother and baby
- Current guidelines and evidence-based medicine in the management of young women in their journey through to motherhood.
Who should watch:
Healthcare professionals with patients living with chronic inflammatory disease including rheumatologists, nurses, GPs, gynaecologists, obstetricians, midwives, pharmacists.
ARMA webinars are free to access thanks to the support of our partners. We would like to thank UCB for supporting this webinar who have had no editorial control/input in its development.
Presenters:
Professor Peter C. Taylor MA, BM, BCh, PhD, FRCP, FRCPE, Professor of Musculoskeletal Sciences, Oxford University;
Professor Catherine Nelson-Piercy MA FRCP FRCOG, Consultant Obstetric Physician, Guy’s and St. Thomas’ Hospitals Trust and Queen Charlotte’s and Chelsea Hospital.
How to integrate mental and physical healthcare for long term musculoskeletal conditions
29 March 2019
The importance of integrating psychosocial care into the treatment of long term musculoskeletal conditions is well established. What would this look like in practice? Using the example of the 3 Dimensions for Long Term Conditions service at King’s Health Partners this webinar covers why and how to provide and effective integrated service which benefits patients and works for clinicians. The 3 dimensions service is not an MSK service, but the approach would work equally well in supporting people with MSK conditions.
Depression is the most common co-morbidity among people with rheumatoid arthritis (RA), and the presence of depression can lead to a person’s pain and overall disability being worse. Yet in a recent survey of people with RA, 2 in 5 had never been asked by a healthcare professional about their emotional or psychological wellbeing. Twenty two percent had a diagnosis of depression, but 37% of these were not receiving treatment for that depression.
The webinar explains why we need to integrate mental and physical healthcare, common psychological reactions and symptoms. It describes an example of psychosocial integration using a stepped care approach and explore the challenges and successes of joint working.
Presenter: Dr. Lindsay Ip, Principal Clinical Psychologist at King’s Health Partners (KHP)
Who should watch: This webinar is for anyone involved in providing or commissioning services for people with long term musculoskeletal conditions.
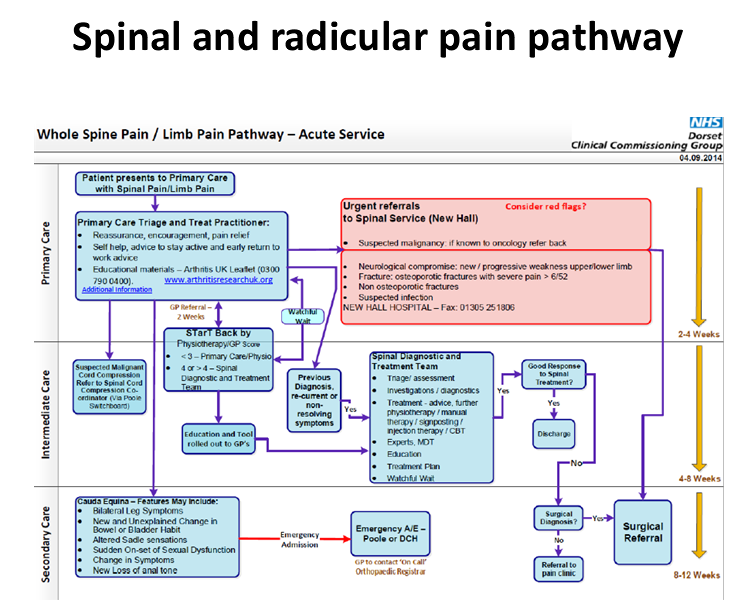
How to implement the National Back and Radicular Pain Pathway (NBRPP)
8 March 2019
The webinar aims to support the implementation of the National Back and Radicular Pain Pathway. It explains the pathway and present data from early adopters to help make the case for change in your local area. The physiotherapist that led the implementation of the NBRPP across Cheshire and Merseyside as part of the Walton Centre Vanguard Project will talk about her experiences, common barriers to implementation and strategies to overcome them.
Back pain is the largest single cause of disability in the UK, with lower back pain alone accounting for 11% of the total disability of the UK population as well as the largest cause of sickness absence.
The NBRPP is the product of a unanimous consensus of 29 stakeholders based on best evidence. Its objectives are to provide a streamlined care pathway for radicular pain and an effective, managed pathway for patients with low back pain. Value impact analysis has indicated substantial cost savings in early implementation in the North East. The Pathway is demonstrating improved clinical results in patient clinical outcomes and patient satisfaction.
Who should watch: All professionals involved in the commissioning and delivery of spinal care.
Presenters:
Stephen Hodges, NHS RightCare
Samantha Davies, The Walton Centre
Everything you wanted to know about setting up a Musculoskeletal Service but were afraid to ask!
15 February 2019
This webinar describes how we set up the Telford Musculoskeletal Service, some of the problems we encountered along the way, and our solutions.
After winning a tender three years ago, the MSK Service was devised to be a single point-of-access for Rheumatology, Pain, Physio, Orthopaedics and musculoskeletal services in the NHS within Telford. The service is a Prime Vendor-type model with Shropshire Community Trust holding the main contract and sub-contracting to other NHS and Private providers in the locality.
Who should watch? Commissioners, First contact practitioners, GPs, hospital consultants, physiotherapists, Patients and Patient Organisations and charities.
Presenters:
Dr Louise Warburton, GPwSI in Rheumatology and Musculoskeletal Medicine at NHS Telford and Wrekin;
Claire Horsfield, Outpatient AHP Service Manager at Shropshire Community Health NHS Trust.
ARMA webinars are free to access thanks to the support of our partners. We would like to thank Roche Products Limited and Chugai Pharma UK for supporting this webinar with an unrestricted independent grant. The pharmaceutical companies have had no editorial involvement in this webinar.
Supporting people with musculoskeletal conditions to be more active
30 November 2018
The benefits of physical activity for musculoskeletal health are well known. Despite this, many people are less active than recommended levels. People with musculoskeletal (MSK) conditions have additional barriers caused by their condition, particularly pain. What can be done to support people to be more active?
Three different initiatives attempt to do just this. Moving Medicine and the Chartered Society of Physiotherapists Love Activity campaign both aim to help supportive conversations with patients about increasing physical activity. parkrun MSK ambassadors aim to provide a safe environment to encourage and support people to walk or run or volunteer at their local parkruns. The webinar looks at how clinicians can encourage and support physical activity and how activity providers can better understand the needs of people with MSK conditions and how to make them feel included.

in partnership with
Arthritis Action
Who should watch? Anyone who works with people with MSK conditions, providers of physical activity and those working in public health.
Presenters:
Dr Ai Lyn Tan
Associate Professor, Honorary Consultant Rheumatologist, UK University of Leeds, Leeds teaching Hospitals NHS Trust, and parkrun Outreach Ambassador Arthritis & Musculoskeletal Conditions, for parkun
Hamish Reid
Sport and Exercise Medicine Consultant, Oxford University Hospitals NHS Trust
Sara Hazard
Assistant Director Strategic Communications, Chartered Society of Physiotherapists
A new way of delivering MSK pain service: Integrated Pain Assessment and Spinal Service
Tuesday 20 November 2018
This webinar describes the Integrated Pain Assessment and Spinal Service (IPASS) which started in 2016 in Berkshire West. We discuss the previous state of pain management in Berkshire West and the reasons for coming together as a system to develop IPASS. The video covers how joint working with a strong patient focus can improve outcomes, and outlines the positive outcomes after IPASS, a services that has been recognised by the British Society for Rheumatology (BSR) for a Best Practice Award in 2016.
Presenters:
Dr. Antoni Chan
Consultant Rheumatologist and Associate Medical Director, Royal Berkshire NHS Foundation Trust
Dr. Rupert Woolley
GP and CCG clinical lead for Planned Care
Anna Wylie
Operational service manager and Extended Scope Physiotherapist, Integrated Pain and Spinal Service
Click here to download the PowerPoint slides for this presentation.
Watch the recording of this webinar in a YouTube window.
The British Society for Rheumatology’s Choosing Wisely UK Recommendations
1 November 2018
Choosing Wisely UK is part of a global initiative which aims to reduce unnecessary tests and treatment by promoting shared decision-making conversations between patients and their healthcare professionals. The British Society for Rheumatology’s (BSR) recommendations were developed in partnership with patients, nurses, and primary and secondary care clinicians.
This webinar outlines the principles of Choosing Wisely UK including a discussion around shared decision making. We describe the process by which the BSR’s recommendations were developed, before discussing each recommendation in turn and what it means for practice.
Who should watch?
Everyone interested in optimising care for people with musculoskeletal problems, including patients, carers, clinicians from primary and secondary care, allied health professionals and commissioners.
Presenters:
Charlotte Sharp, Rheumatology Specialist Trainee, HEE(NW) and Clinical Academic Fellow, NIHR Collaboration for Leadership in Applied Health Research and Care Greater Manchester
Lizzie MacPhie, Consultant Rheumatologist, Lancashire Care NHS Foundation Trust, and Chair of the British Society for Rheumatology’s Standards, Audit and Guidelines Working Group.
Click here to download the PowerPoint slides for this presentation.
Twitter:
@sharpcharlotte and @lizzymacphie
Commissioning for Quality: Community-based Rheumatology Service
19 October 2018
The webinar outlines how a community-based rheumatology service can provide effective management of rheumatology patients, with benefits both to the patients and the usage of clinical resources. The Service is commissioned by the CCG and GPs from participating practices refer directly into the Community service.
The service was initially established in 2009 by a GPWSI who had 10 years + working in a secondary care rheumatology service as a clinical assistant, together with a nurse consultant in rheumatology with over 20 years’ experience.
Findings from the pilot study demonstrated that patients requiring disease-modifying anti-rheumatic drugs (DMARDS) can easily be managed in a community setting. A community setting with provision of the specialist skills provides patients with local, more convenient care and reduced disengagement. It also optimised the use of local resources – for example, moving some of the routine follow-up activity for rheumatology patients (such as drug monitoring) would undercut the tariff by 30%. Patients see the most appropriate member of the healthcare team allowing more effective management of their condition and freeing up specialist rheumatologists for more acute cases.
The service now has 3 GPWSI, 1 extended scope physiotherapy practitioner, 2 nurse consultants and a clinical nurse specialist, as well as 6 consultant sessions per month plus 2 full time administrators.
Presenter:
Erica Gould, Nurse Consultant at Community Rheumatology Service Modality Partnership
Who is this for? Commissioners, GPs, clinicians working in rheumatology services.
Click here to download the PowerPoint slides for this presentation.
Watch the recording of this webinar in a YouTube window.
Focus on Musculoskeletal Health: developing and implementing a JSNA chapter
6 April 2018
As a group musculoskeletal conditions cause 31.3% of all years lived with disability, and their incidence is rising as the population ages. Understanding this at a local level is therefore crucial in public health, prevention and health and care provision. With an ageing population this becomes increasingly important for a healthy workforce and a strong economy.
This webinar was one of a series delivered in partnership between the Arthritis and Musculoskeletal Alliance (ARMA) and NHS England. Using the example of the London Borough of Ealing and NHS Ealing CCG, the webinar outlined the development of the JSNA chapter and why this is important for improving the musculoskeletal health of a local population.
The JSNA is a statutory document that describes the health and social care needs of the population, identifies gaps and unmet needs, and makes evidence-based recommendations to health and social care commissioners.
Presented by:
Ian Bernstein, Clinical Lead for Musculoskeletal Transformation, NHS Ealing CCG and NW London STP Rutuja Kulkarni-Johnston, Consultant in Public Health, London Borough of Ealing
Professor Kevin Fenton MD PhD FFPH, Director of Health and Wellbeing, Southwark Council
Download the slides for this webinar in PDF format.
Sport, Exercise and Musculoskeletal Training and Delivery in the NHS
Friday 8 September 2017
Presented by Natasha Jones, Consultant in Sport and Exercise Medicine, Nuffield Orthopaedic Centre, Oxford University Hospitals NHS trust and Mike Rossiter, Consultant in SEM & MSK Lead, Hampshire Hospitals NHS Foundation Trust
The webinar gives a brief outline of the Faculty of Sport, Exercise and Musculoskeletal Medicine (FSEM), particularly it’s aims and what the speciality covers. It also details the scope of work of a Sport & Exercise (SEM) Consultant, both within and outside of the NHS. It will highlight the particular importance of Exercise medicine within the Health of the Nation and the potential for this area of medicine.
There is an example of how an NHS Musculoskeletal (MSK) service has been set up and run successfully and the positive impact it has on investigations and interventions.
Finally, the webinar outlines current SEM training and accreditation within the UK.
This webinar is aimed at NHS Trusts (or other bodies) that are thinking of setting up, or refining, an MSK service, and professionals who wish to find out more about the FSEM, particularly those that are considering following this speciality as a career.
To watch the webinar recording, click here.
Self-care and prevention workforce skills and competencies webinar
presented by Beverley Harden, Associate Director of Education & Quality, South, HEE
28 April 2017
“A radical upgrade in prevention” “changing the relationships with people and communities”
(FYFV 2014)
 HEE is working with and across the system to articulate how we develop the workforce to build skills in person centred approaches, i.e. how we work in partnership with people and their families to support health and wellbeing. This work brings together the core skills of:
HEE is working with and across the system to articulate how we develop the workforce to build skills in person centred approaches, i.e. how we work in partnership with people and their families to support health and wellbeing. This work brings together the core skills of:
- health coaching
- care and support planning
- shared decision making
- a number of behavioural change interventions
The work illustrates the values, strengths based approach and core skills to enable the workforce to more consistently build relationships and partner with people to support effective prevention (at all levels from obesity to loneliness to medicines compliance) and self-care/management.
The webinar discussed the thinking to date, considered some areas where the techniques have been utilised and the impact they have had for people, both patients and staff. The conversation then explores the ‘how’: how we shift thinking for services and busy people from reactive to preventative, how we skill people to habitually work in this way and support their own behaviour change in service.
Stream: Self-care workforce skills
Stream: Q&A
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: Self-care workforce skills
Download and keep: Q&A
Joint Pain Advisor Webinar by London Health Innovation Network
24 March 2017
Chronic joint pain accounts for around 1 in 5 primary care consultations. GPs feel overwhelmed and are concerned that they don’t have the time or the skills to give people adequate information or advice about exercise and weight control (NICE core recommendations).
To improve access to better management London Health Innovation Network has introduced Joint Pain Advisors into six primary care surgeries. Their role is to give people simple information, advice about self-management strategies, constructed personalised care plans and use behavioural change techniques to help people adopt healthier lifestyles. Patients were reviewed at 3 weeks, 6 weeks and 6 month intervals, at which the Advisor fed back progress, reinforced health messages and provided on-going support, reassurance and encouragement where required.
Over 500 patients used this service and reported less pain, better function and higher activity levels. A high satisfaction rate was achieved which included reduced BMI, body weight and waist circumference and has led to fewer GP consultations, investigations and onward referrals.
The Joint Pain Advisors role has been enthusiastically accepted and is a more effective, efficient and sustainable way to deliver care to this high proportion of people.
Stream slides and commentary: Joint Pain Advisor presentation
Stream: Q&A
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: Joint Pain Advisor presentation
Download and keep: Q&A


Getting It Right First Time (GIRFT) Masterclass
10 March 2017
Getting It Right First Time – reducing unwarranted variations
Getting It Right First Time (GIRFT) is a national, clinician-led programme, created to help improve the quality of medical and clinical care within the NHS by identifying and reducing unwarranted variations in service and practice. Following a successful pilot in orthopaedics, led by Professor Tim Briggs of the Royal National Orthopaedic Hospital, GIRFT has received £60m of Government funding and is now being rolled out to more than 30 specialties including neurosurgery, emergency medicine and cardiothoracic surgery.
This webinar explores the philosophy behind GIRFT, its methodology, including the deep dive data analysis and peer-to-peer engagement with frontline medics, and importantly the benefits it has brought in improving patient outcomes and delivering efficiencies through the sharing of best practice.
Trusts involved in the pilot programme have already reported direct savings and benefits of between £20m and £30m, with an additional £15m to £20m expected in the second year. At the end of GIRFT’s three year funding it is expected that the programme will have helped prevent £1billion of wasted costs and unnecessary treatment.
The webinar was jointly presented by Rachel Yates, Managing Director of GIRFT, and Mary Newman, Interim Head of Policy and Implementation GIRFT. It will be of interest to Health Care Professionals and Commissioners from CCGs, Primary & Secondary Care and Clinicians.
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: Getting it Right First Time webinar and Q&A
Webinar – MSK Clinical Networks
Dr Ian Bernstein, NHS Ealing CCG, 29 April 2016
Clinical Networks: Transforming Musculoskeletal Care in North West London. To open the narrated slide presentation (powerpoint with audio), please click below.
Learning objectives, programme and more details are available on the MSK Knowledge Network on Yammer. Please see the “Useful Documents, Tools and Files” section. You can also find the full video version of this presentation and slides-only version there.
Webinar – Physiotherapy in Primary Care
Q&A with Andy Lord, 21 June 2016
Presentation on MSK Physiotherapy in Primary Care (Self-Referral to Colocation) led by Chartered Society of Physiotherapy (CSP).
Click image to open presentation on Prez.com.

The Musculoskeletal Health Questionnaire
24 February 2017
Musculoskeletal disease (MSK) is one of the largest single sources of disability in the UK and MSK services are making major changes to address growing demands.
To date few direct measures of health status have been in place which could be used across the spectrum of MSK to inform service improvement. The introduction of the Musculoskeletal Health Questionnaire (MSK-HQ) has been developed to meet this need. The webinar will introduce different possible applications from audit, quality improvement and performance evaluation through to facilitating communication and personalised care with individual patients. The role of Patient Reported Outcome Measures (PROMs) will also be discussed.
The webinar was presented by Raymond Fitzpatrick, Professor of Public Health and Primary Care and Elizabeth Gibbons, Senior Research Scientist both from the University of Oxford who provided an overview of their experiences and plans for use of MSK-HQ in various NHS settings. This webinar will be of relevance to any health professional, manager or commissioner concerned with MSK service provision.
Stream: The Musculoskeletal Health Questionnaire webinar
Stream: The Musculoskeletal Health Questionnaire Q&A
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: The Musculoskeletal Health Questionnaire webinar
Download and keep: The Musculoskeletal Health Questionnaire Q&A
Presented by Christian Verrinder and Giles Hazan
10 February 2017
Dr Christian Verrinder and Dr Giles Hazan share aspects of their experience to date in MSK commissioning, including their thoughts on: process, structure, design, procurement, implementation and review.
This webinar looks at how we can build on current service provision for people with MSK conditions in order to identify how and where current services and support can be improved and reflects how this new programme of work has influenced the commissioning of MSK services.
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: New models of MSK Masterclass webinar
Download and keep: New models of MSK Masterclass Q&A

Lead by Tony Woolf in participation with ARUK/BSR
12 January 2017
The Musculoskeletal Health in the Workplace Project aims to prevent work loss caused by musculoskeletal problems.
In 2013 31 million lost workdays in the UK were attributed to musculoskeletal conditions, compared with 27 million for minor illnesses like coughs and colds and 15 million for stress and anxiety. We are all living longer and working longer so we need a system that promotes economic independence, health and wellbeing and productivity throughout life.
The Musculoskeletal (MSK) Health in the Workplace Project aims to prevent work loss caused by musculoskeletal problems. There has been much focus on health protection but the problems remain. There is a need for a different approach that brings together health promotion and health protection along with health management with a focus on being proactive rather than reactive; enabling managers and employees to achieve this; and empowering people to and self-manage their MSK condition.
The management of MSK problems needs to focus on getting people back to functioning in order for them to stay in or return to work. Early intervention, rehabilitation and return to work support are all ways of achieving this.
This webinar looked at how we can build on the current service provision for people with MSK conditions in order to identify how and where current services and support can be improved.
It was presented by Professor Tony Woolf, Consultant Rheumatologist and Honorary Professor of Rheumatology, University of Exeter Medical School, and Plymouth Peninsula Medical and Dental College. The webinar was produced in participation with Arthritis Research UK and the British Society for Rheumatology, targeting a specific audience of MSK professionals, Occupational Health leads, GPs and CCG Commissioners.
Stream: Work & Health MSK webinar
Stream: Work & Health MSK Q&A
The following downloadable versions can be kept for offline viewing with the Webex Player:
Download and keep: Work & Health MSK webinar
Download and keep: Work & Health MSK Q&A

Webinar Specifically for Users of Musculoskeletal Health Services
Government Green Paper on Work & Health
Friday 27 January 2017
Building on the current service provisions for people with Musculoskeletal conditions.
We are pleased to be able to share the news that ‘Improving Lives – the Work, Health and Disability Green Paper’ was published on the 31 October 2016 by the Department for Work and Pensions and the Department of Health and reflects the Government’s new and ambitious approach to work, health and disability.
We want to spark a far-reaching, national debate on the issues and the proposals set out in the document, ensuring that we listen to you so that we can develop our programme of work and understand the role others have to play in driving action forward.
How can you as a service user be involved and help shape your future services?
The Work and Health Unit would like to work closely with people working in or needing Musculoskeletal services in order to identify how and where current services and support can be improved, as we start developing policy proposals for improving MSK services for both service users and professionals.
Looking widely across the current range of services and provision of support for people with MSK, we would like to discuss with service users your views on these questions:
- how do you access MSK services and how can this access be improved?
- how can you be assisted to stay in work/return to work after being away from work due to your condition?
- how can practitioners (non-specialist health, employability professionals, work coaches) help you with work and health issues?
- how MSK services can provide you with the help and care you need and link with employment support to deliver a more joined-up service for you.
This webinar was part of a public consultation which ran until 17th February 2017.
‘Improving Lives – the Work, Health and Disability Green Paper’ can be found at http://www.gov.uk/
MSK webinar series: Designing Optimal Falls Services webinar
Friday 7th July 2017
Falls and fractures are a common and serious health issue. The human cost can include distress, pain, injury, loss of confidence, loss of independence and mortality. For health services they are both high volume and costly with 255,000 falls related emergency hospital admissions per year for older people in England and the annual cost of hip fractures to the UK estimated at being around £2 billion.
RightCare is a national programme to improve population health by addressing unwarranted variation. In collaboration with national experts and patient groups, is launching an ‘Optimal Solution for Falls and Fragility Fractures’ to support systems to improve outcomes.
In January, a number of national organisations launched a ‘Falls and fragility fractures consensus statement’ and we are now publishing an accompanying technical annexe with resources to support delivery of key interventions and the RightCare Optimal Solution.
The webinar will introduce the Falls and Fragility Fractures Optimal Solution and how this is supported by the new technical annexe. This will assist health economies in the delivery of key interventions including how to develop a fracture liaison services according to clinical standards as well as strength and balance exercise programmes. For those with established services, this is an opportunity to ensure that your service is optimally configured for your population.
This webinar will be presented Amy Bowen, Optimal Solutions Lead NHS RightCare, Daniel MacIntyre, Population Health Services Manager, Public Health England, Tim Jones, from National Osteoporosis Society and Ann Parry, living with osteoporosis and will be of relevance to any health professional, manager or commissioner concerned with improving Falls and Fragility Fracture Services.