 MSK First Contact Practitioner roles; are they fit for the future for Primary Care?
MSK First Contact Practitioner roles; are they fit for the future for Primary Care?
by
Amanda Hensman-Crook FCSP, HEE AHP National Clinical Fellow, Consultant MSK Physiotherapist
Neil Langridge FCSP, Consultant MSK Physiotherapist
Laura Finucane FCSP, MSK Consultant MSK Physiotherapist
Chris Mercer FCSP, MSK Consultant MSK Physiotherapist
MSK First Contact Practitioner roles and the advancing practice agenda is moving at pace and as a result, there has been some anxiety around the MSK First Contact workforce. This has been expressed about several aspects of the roles, including:
- numbers needed to ensure sustainability without wider destabilisation of the MSK workforce
- where the workforce will come from with the requisite capability
- concern about governance of the roles
- who provides the supervision and support
- a general need to understand the offer of the role to primary care
- concern from other MSK professions that they are not included in the GP contract reimbursement scheme (DES) and where they might fit in the bigger picture.
Work is being done collaboratively with Health Education England (HEE), NHS England (NHSE) and NHS England Improvement (NHSEI) to address all of the above to ensure that the education, governance, supervision, strategy and infrastructure is in place to ensure a sustainable model of MSK care at the front of the care pathway.
Standards
Quality and governance are key to first contact roles. To ensure this, the right capabilities at the right level need to be credentialed and accredited. The minimum requirement for a first contact role is to be working at an advanced level clinically i.e. at level 7 (masters level). It is desirable that the clinician who meets that criteria is also on the Advanced Clinical Practice pathway (ACP) to fulfil level 7 across all four pillars – clinical, education, research and leadership.
In physiotherapy, an important step has been taken with an agreement on a national UK standard across all MSK speciality groups. A piece of work was undertaken by Birmingham University that has led to this agreement, funded by HEE, which cross referenced the International Federation of Orthopaedic and Manipulative Physiotherapists (IFOMPT)* standards against the multi-professional
The outcome of this exercise demonstrated that the two frameworks aligned with the IFOMPT standards. These findings are significant as the IFOMPT standards are already used in Higher Education Institutions (HEIs) leading to Musculoskeletal Association of Chartered Physiotherapists (MACP) membership, along with the HCPC standards to examine clinicians against a level 7 framework. This agreement is central to an educational roadmap from graduate to level 7 to credential a portfolio route in the workplace to Advanced Clinical Practice.
For physiotherapy this standard is now set, but the vision is to create a common MSK standard across all MSK professions that will assure the system of advanced practice in the UK.
This will be achieved by cross referencing other MSK professional standards against the updated IFOMPT standards and making any changes, if needed, to accommodate any gaps. The outcome will be that education in MSK to advanced practice in the UK will be standardised, and all professions will be able to sit on the MSK educational roadmap to develop their career pathway.
Education
Educational Roadmap
To create an MSK pathway from graduation to level 7 Advanced Clinical Practice, a roadmap is being developed. This will provide educational support that will aid clinicians in identifying learning opportunities in the workplace, gaining advanced skills and knowledge, and generating knowledge from reflective practice. It will give clear guidance of what competencies need to be achieved at each level, and ways on how to evidence this. Ultimately this will support different routes including an equivalence (portfolio) route to Advanced Clinical Practice from graduation over an expected minimum of 5 years.
Portfolio sign off to clinical level 7 in the workplace
FCP roles have a minimum requirement of advanced (level 7) sign off in the clinical pillar of ACP. Outside the HEIs, the development of a portfolio supported by HEE to advanced clinical practice incorporating mandatory primary care learning is underway which will be held by the APPN. This can be adopted by all MSK professions. Capability sign off will be carried out by both the clinical supervisor in the workplace and the clinician who will sign against a declaration to their professional registration.
Higher Education Institutions (HEIs) and professional special interest groups
There is a lot of work going on in the development of courses in universities (HEIs) across England and within MSK special interest groups linked to HEIs to develop level 7 FCP standalone modules and ACP Master’s degrees.
To make the ACP Masters easier to develop and to tailor to a specific profession or speciality, the overarching core generic capabilities are being mapped by HEE from the multi professional ACP framework. The capabilities specific to primary care for FCP modules on top of the already defined core, are also being identified. This will give a central minimum requirement for HEIs to build advanced practice Master’s degree courses from and enable them to pull stand-alone level 7 modules such as a First Contact Practice module or MSK module into an ACP course to tailor to the specific need of the clinician.
The taught level 7 First Contact stand-alone modules teach the nuances of working in primary care, largely modelled around the eight CPD modules in the Health Education England’s MSK primary care e-learning. The e-learning modules cover: What is primary care, identification of the ill and at risk, mental health in primary care, complex decision making, public heath, persistent pain, overview of medicines and prescribing and serious pathology of the spine.
These e-learning modules are a minimum requirement for a clinician who is already working at clinical level 7 outside primary care to prepare for an FCP role and are free CPD to all in the NHS and can be bought outside the NHS to complete.
To support upskilling MSK clinical capabilities for all MSK professions to clinical level 7 (advanced level) the Society of Orthopaedic Medicine has now opened all their courses out to all MSK clinicians, and the Musculoskeletal Association of Chartered Physiotherapists are developing their course curriculum further to be a vehicle for advanced practice educational sign off as well as signing off at level 7 via the equivalence (portfolio) route, and in-house FCP modules.
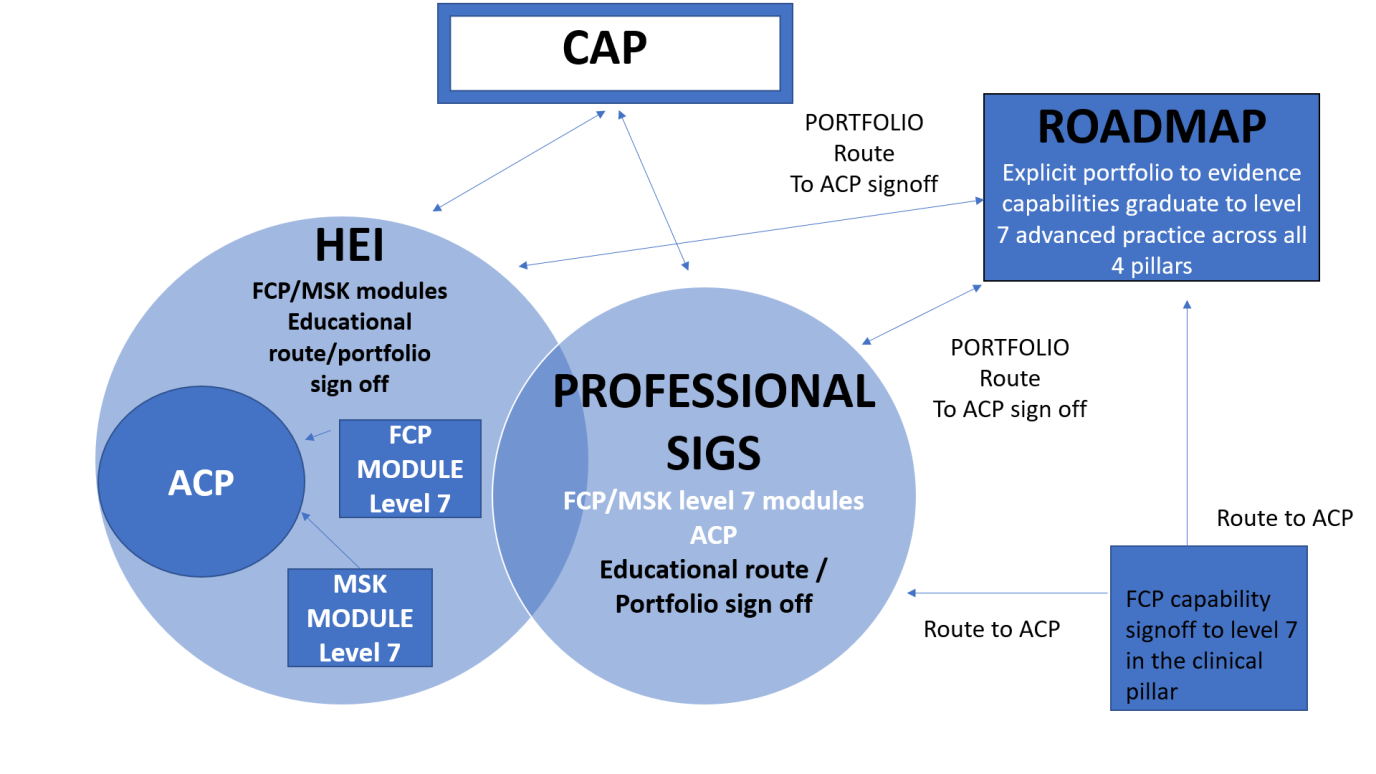
The diagram below provides a visual diagram of where FCP sits and the routes to ACP. CAP is the Centre of Advanced Practice that sits in HEE.
Supervision
To support clinicians, there is a need for supervision for both clinical work and CPD. In primary care day to day clinical supervision is to be provided by a named supervisor at the GP practice. CPD supervision is to be provided by the Trust or private provider with the exception of an individual directly employed by a Primary Care Network (PCN) who needs to be supervised by the PCN.
There is an Advanced Practice supervision framework coming out soon to support this.
Further information
For further information with links to a timeline and FCP papers and resources, please refer to this paper: ‘A retrospective review of the influences, milestones, policies and practice developments in the First Contact MSK model’, Langridge, Hensman-Crook 2020, https://arma.uk.net/wp-content/uploads/2020/05/FCP-MSK-review-with-authors_v3.pdf
*(IFOMPT is an international body of 22 national groups who are clinical experts in MSK)