 In what is very likely to be an election year, National Voices have shared their Manifesto for Equitable Healthcare – which puts forth three general election priorities.
In what is very likely to be an election year, National Voices have shared their Manifesto for Equitable Healthcare – which puts forth three general election priorities.
Co-produced with National Voices’ members, the manifesto is supported by a common theme – ensuring that the NHS works for all, not just those who know how to navigate the system or who come from more privileged backgrounds.
The manifesto seeks to remind politicians that adopting these priorities will not just improve things for patients but will also help drive NHS stability and wider economic benefits.…
Read more of this article



 by Sue Brown, CEO ARMA
by Sue Brown, CEO ARMA

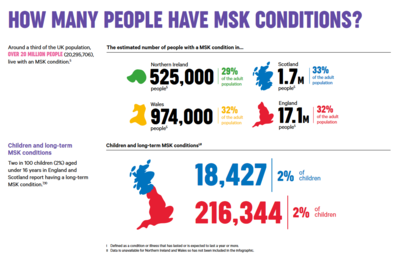
 The government has announced ambitious plans to get an additional 3.5 million people physically active by 2030. The announcement was accompanied by the publication of a report,
The government has announced ambitious plans to get an additional 3.5 million people physically active by 2030. The announcement was accompanied by the publication of a report,