The UK MSK Advanced Practice Standards:
What are they and what purpose do they serve?
What are the UK Musculoskeletal Advanced Practice Standards?
The United Kingdom Musculoskeletal (MSK) Advanced Practice Standards (the Standards) outline the minimum knowledge, skills and behaviours required of clinicians working at advanced practice level in the UK within the MSK specialty, across professions and sub-specialties. They are designed to inform and underpin the development and delivery of MSK advanced practice education and training programmes and pathways across the UK (at academic level 7/11; (Master’s degree level).
The Standards can be found here.
What is Advanced practice?
Advanced practice is where a clinician has proven capability across the four pillars of practice: Clinical, Leadership and Management, Education and Research at master’s level (academic level 7/11) both academically and with the application of academic knowledge into practice. They work multi-professionally and cross organisationally providing systems leadership.
Why were the Standards developed?
The Standards were developed to support and promote advanced education and practice in MSK and to reduce unwarranted variation in education and practice across the regulated MSK professions and sub-specialties. In so doing, their additional purpose is to enhance the quality of MSK care, uphold patient and clinician safety, and strengthen system-level leadership to benefit populations, patients and services.
Who were the Standards developed by?
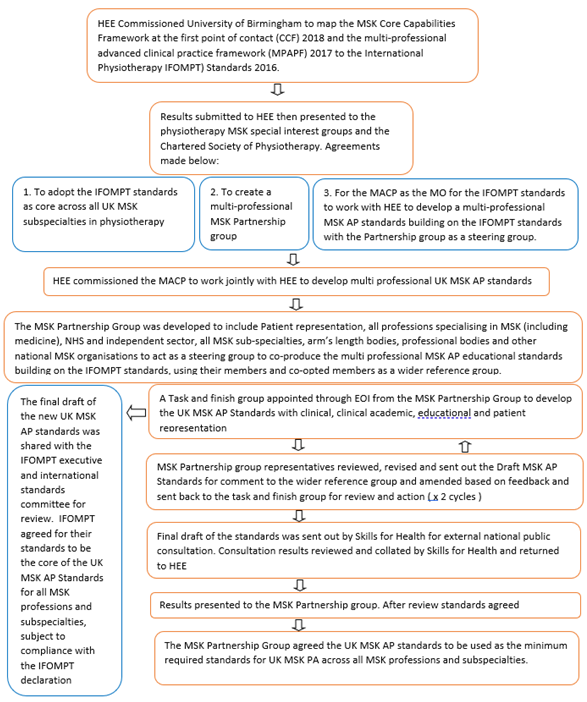
The Standards were co-produced via the UK MSK Partnership Group. The Group has broad representation from patient groups/individuals with lived experience, professions specialising in MSK (including medicine), MSK sub-specialties, government arm’s length bodies, professional bodies and other national MSK organisations.
How were the Standards developed?
The UK MSK Partnership Group formed a task and finish group to draft the Standards, with the MSK Partnership Group acting as a steering group to oversee the document’s development. Draft versions of the Standards were shared for comment with a reference group. The reference group comprised the Partnership Group’s member organisations, with co-optees to broaden input. A wider national opportunity to feed back on the draft was provided via Skills for Health’s online consultation platform.
It was agreed by the MSK Partnership Group that the standards of the International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) standards (2016) should form the core on which the UK Standards were built.
Permission was gained from IFOMPT to use its standards in this way. The IFOMPT statement indicating that this permission was granted is included in the Standards.
The process and governance arrangements for the Standards’ development are outlined in the appended chart.
Are the Standards relevant to all four nations?
The Standards were co-produced with representation from all four nations of the UK, with the intention that they should have UK-wide currency. By defining the minimum knowledge, skills and behaviours required of MSK advanced practice, they should inform and underpin the design and delivery of education and training programmes and development pathways (e.g. MSc programmes and portfolio routes) in each nation.
What do the Standards mean to different stakeholder groups?
- Public and patients: the Standards should assure the public and patients that MSK practitioners working at advanced practice level have developed and demonstrated the minimum professional capabilities to work safely and effectively at this level of practice.
- Clinicians: the Standards should provide clarity to individual practitioners and teams about the minimum knowledge, skills and behaviours that they need to develop, demonstrate and maintain to practise safely and effectively at advanced practice level in MSK and its sub-specialties.
- Service managers/service providers: the Standards clarify the minimum knowledge, skills and behaviours that all MSK practitioners need to hold and maintain to practise at advanced practice level, thereby supporting workforce deployment and flexibility and reducing unwarranted variation in practice.
- Commissioners: the Standards clarify to commissioners the minimum knowledge, skills and behaviours required of advanced practice MSK education, practice and service delivery, with these minimum requirements then logically reflected in system-level planning and specifications to meet population, patient, service delivery and workforce development needs.
- Education providers: the Standards should inform and underpin education providers’ development and delivery of MSK advanced practice education and training programmes and development pathways, thereby contributing to assuring the quality of learning experience and outcomes and reducing unwarranted variation across provision.
England-specific questions
Do the Standards map to the generic capabilities in the multi-professional advanced practice framework of Health Education England (HEE)?
The Standards map to the generic capabilities set out in HEE’s 2017 Advanced Practice Multi-professional Framework. The mapping to the IFOMPT standards (2016), as the UK MSK AP Standards’ core, to the Framework is published in a peer-reviewed journal (Noblet et al, 2021).
How do the Standards relate to the MSK roadmap for becoming a first-contact practitioner in England?
The knowledge, skills and attributes (KSAs) in the MSK Roadmap defined for MSK first-contact practitioner roles are the clinical component of the Standards. The Roadmap KSAs align with the capabilities in the clinical pillar of HEE’s advanced practice framework with the exception of medical complexity.. The KSAs align with some of the capabilities within the other three pillars of advanced practice.
How is an HEE credential due to link with the Standards?
HEE’s Centre for Advancing Practice is overseeing the development of multi-professional advanced practice credentials for use in England. A Credentials’ purpose is to develop advanced practice workforce capability and capacity to meet high-priority population, patient, system-level and service delivery needs. Centre-endorsed credential specifications define the advanced practice capability and learning and development requirements in particular areas of practice. They are designed to be implemented within advanced practice education and training provision and to underpin targeted financial support for advanced practice workforce development.
In line with their defined purpose, the UK Standards are currently forming the basis for developing an MSK credential specification for use in England.
Appendix – Process and governance arrangements for the Standards’ development