 The importance of exercise when living with inflammatory arthritis
The importance of exercise when living with inflammatory arthritis
Live discussion with expert panel on the importance of exercise when living with inflammatory arthritis.
Facebook Live event
Wednesday, 29 March 2023, 7pm
Exercise doesn’t need to be all lycra and gym equipment! There are so many ways to keep those joints, tendons, muscles moving, so join NRAS live on Wednesday, 29 March at 7pm to hear more about yoga, resistance training, team sports and more, as well as how to overcome some of those hurdles (not literal ones!)…
Read more of this article


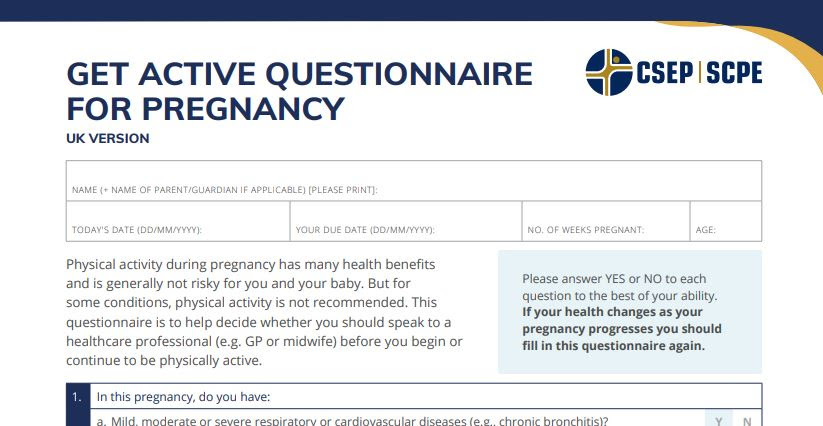 Sport Rehabilitator Marlize De Vivo collaborated with this effort which recognises the importance of continued physical activity and acknowledges the role of healthcare and qualified exercise professionals in facilitating an active pregnancy:
Sport Rehabilitator Marlize De Vivo collaborated with this effort which recognises the importance of continued physical activity and acknowledges the role of healthcare and qualified exercise professionals in facilitating an active pregnancy:

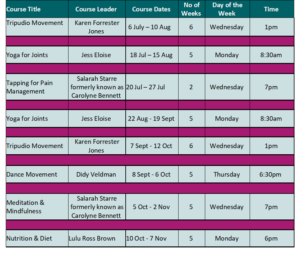
 Looking differently at leisure places as spaces for chronic pain management
Looking differently at leisure places as spaces for chronic pain management


 Physiotherapist Katie Knapton from PhysioFit and Pete Moore from the PainToolkit have co-written a self-management guide for people suffering with Long Covid. This is free and entry-level information to try and help people on the path to recovery.
Physiotherapist Katie Knapton from PhysioFit and Pete Moore from the PainToolkit have co-written a self-management guide for people suffering with Long Covid. This is free and entry-level information to try and help people on the path to recovery.
 New consumer research from the British Chiropractic Association (BCA) reveals that 52% of people across the UK are planning to use digital fitness solutions to stay fit and healthy as lockdown restrictions lift.
New consumer research from the British Chiropractic Association (BCA) reveals that 52% of people across the UK are planning to use digital fitness solutions to stay fit and healthy as lockdown restrictions lift.

 Versus Arthritis has launched a new free physical activity programme, Let’s Move with Leon, designed and presented by exercise expert Leon Wormley who specialises in working with people with arthritis and related conditions. The programme consists of weekly 30-minute movement sessions delivered right to a subscriber’s email inbox. Leon’s classes are a holistic, full-body programme and – they’re great fun!
Versus Arthritis has launched a new free physical activity programme, Let’s Move with Leon, designed and presented by exercise expert Leon Wormley who specialises in working with people with arthritis and related conditions. The programme consists of weekly 30-minute movement sessions delivered right to a subscriber’s email inbox. Leon’s classes are a holistic, full-body programme and – they’re great fun!