
 Reflection from the national clinical co-leads for the Welsh national musculoskeletal clinical Network
Reflection from the national clinical co-leads for the Welsh national musculoskeletal clinical Network
Dr Meinir Jones, General Practitioner, Associate Medical in HDUHB;
Dr Rob Letchford, Consultant Physiotherapist MSK rehabilitation in CAVUHB
Six months into these new roles, we find ourselves reaching a peak of optimism and enthusiasm for the future. In the aftermath of a devastating two years that has negatively affected so many, and left previously stretched health services with unprecedented challenges, that seems a ridiculous position to hold. Perhaps it’s our optimism (given the positive effects on health we recommend that you try it out too!).…
Read more of this article


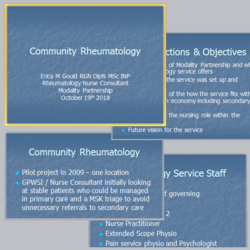
 Musculoskeletal support professionals in the community
Musculoskeletal support professionals in the community


 You can now see the video from our recent webinar in the Musculoskeletal Networks series:
You can now see the video from our recent webinar in the Musculoskeletal Networks series:
 The video of the latest webinar in the MSK Webinar Series is up on our site.
The video of the latest webinar in the MSK Webinar Series is up on our site.